Getting to know your menstrual cycle, allows you to understand the pattern of events that take place in your body, each cycle.
Knowing how long your cycles are, when you're fertile and when you ovulate will help you achieve your goal of getting pregnant or avoiding pregnancy.
What is the menstrual cycle?
The menstrual cycle is a cycle of changes that your body goes through as it prepares to conceive each cycle.
This includes building a uterine lining for a fertilized egg to implant and begin growing; releasing an egg to be fertilized, and shedding the uterine lining if the egg is not fertilized. These changes collectively are called the menstrual cycle and are controlled by hormones.
All about cycle lengths
The terms menstruation and menstrual are derived from the Latin word for month, which in turn relates to the Greek word mene, meaning moon. There is much written historically describing menstruation and how it is believed to coincide with the new moon.
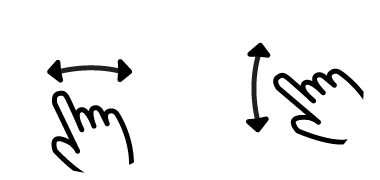
The average menstrual cycle length is 28 days, but they can vary in length from 23 days or less in a short cycle, to over 35 days in a long cycle.
Day one of your cycle is the first day of your period and this continues right up to the day before your next period.
Here is something you may not know... Most women ovulate 15 days BEFORE their next period. How is this so?
The menstrual cycle is divided into phases (more detail on this later), the phase before ovulation, the follicular phase, varies in length from women to women and can even vary for the same women, varying from about 13 to 20 days long.
However, the phase after ovulation, the luteal phase, is the same for most women (12 to 16 days long with the average being 14), and stays consistent for the same women.
Quick overview of how hormones control your cycle
Your menstrual cycle is under the control of two very important structures in your brain: the 'hypothalamus' and the 'pituitary gland'. Here is a quick overview of what happens...
- Your 'hypothalamus' produces Gonadotropin Releasing Hormone (GnRH) at the beginning of each cycle.
- GnRH acts on your 'pituitary gland' to produce Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH).
- LH & FSH then travel to your ovary to induce ovulation. After ovulation they cause the empty follicle to release Estrogen and Progesterone.
- Estrogen and Progesterone make your uterus lining moist and thick, in preparation for implantation of a fertilized egg.
I'll be covering the details of what happens during the menstrual cycle, but if you would like to know more about hormones specifically, click here.
As well as controlling what happens during your menstrual cycle, your hormones can also impact your mood. Some women experience extreme mood changes throughout their cycle and some may not really notice any fluctuations.
Follicle Stimulating Hormone (FSH) which in turn stimulates the ovary to develop egg follicles. As these follicles grow and start to mature, they produce the hormone oestrogen. Just before the middle of the cycle oestrogen levels start to rise. This causes a sudden increase in Luteinising hormone (LH). The rise in LH triggers the rupture of the maturing follicle and releases the egg at ovulation. The egg only lives for a maximum of 24 hours and most likely only as short as 12 hours. The hormone progesterone then kicks into action. If conception does not occur, the levels of progesterone will fall just before the next menstrual period.
Phases of the menstrual cycle
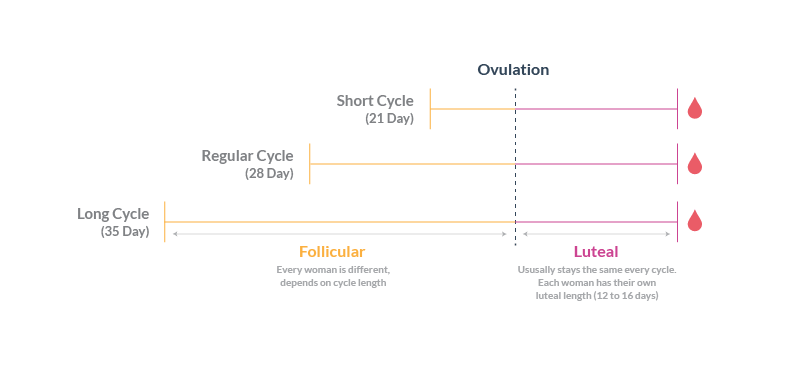
The menstrual cycle can be described as a series of events that happen in the uterus AND ovary. These are known as the Uterine Cycle and Ovarian Cycle. Each of these cycles have three phases:
- Uterine Cycle Phases: MENSTRUAL > PROLIFERATIVE > SECRETORY
- Ovarian Cycle Phases: FOLLICULAR > OVULATION > LUTEAL
See the table below to learn more about the phases. Being aware of these events can help you know when your are most fertile and help you get pregnant.
The following table shows the series of events in a typical 28 cycle. Note: If you have a shorter or longer cycle, the length of the phases before ovulation will be shorter/longer.
| Cycle Days | Uterine Cycle Phase | Ovarian Cycle Phase |
| 1-5 | MENSTRUAL PHASE: Your uterus shreds the lining (endometrium) that was built in the previous cycle in preparation for a new lining. | FOLLICULAR PHASE: A few follicles (nurturing capsule containing undeveloped egg) are stimulated by LH and FSH to grow in the ovary. One will become the dominant follicle that will release an egg during this cycle. The others will stop growing. See follicle development. |
| 6-12 | PROLIFERATIVE PHASE: Estrogen and Progesterone make your uterus grow a new lining. | FOLLICULAR PHASE: Estrogen causes the dominant follicle to continue to grow, it quickly grows in size. Estrogen also causes your cervix to change and produce cervical mucus. |
| 13-14 | PROLIFERATIVE PHASE: Your new uterus lining (endometrium) continues to grow. | OVULATION PHASE: Rising levels of Estrogen trigger a surge of LH which provides the egg in the follicle with a final push to mature before it's released (ovulation). |
| 15-20 | SECRETORY PHASE: Progesterone causes the endometrium to thicken in preparation for possible implantation of a fertilized egg. | LUTEAL PHASE: After ovulation the egg moves down the Fallopian tube towards the uterus. The empty follicle (now called the corpus luteum) stays in the ovary and produces Progesterone. Progesterone is also responsible for your Basal Body Temperature to rise. |
| 21-28: If the egg was not fertilized | SECRETORY PHASE: Progesterone levels drop; the endometrium starts to break apart until it can no longer support itself. The endometrium is then shed again (beginning of a new cycle). | LUTEAL PHASE: The corpus luteum stops producing Progesterone. |
| 21-28: If the egg was fertilized | SECRETORY PHASE: About 8 days after ovulation the fertilzed egg attaches itself to the wall of the uterus (this is called implantation). | LUTEAL PHASE: The corpus luteum receives 'human Chorionic Gonadotropin' hormone (hCG) from the embryo. hCG makes the corpus luteum keep producing Progesterone for about 8 more weeks, after which time the placenta takes over Progesterone production throughout pregnancy. |
More about the luteal phase
After ovulation, the remains of the dominant follicle (that released the egg), transforms into the corpus luteum. The corpus luteum starts to produce significant amounts of hormones, particularly Progesterone. The hormones maintain the thickened lining of the uterus, waiting for a fertilized egg to implant. If implantation does not occur, the corpus luteum withers and dies which causes Progesterone levels to drop, this then causes the uterus lining to break up resulting in menstruation, and so a new cycle begins.
Calculating your luteal phase length
Your luteal phase begins on the day after you ovulate, and runs through the rest of your menstrual cycle, ending the day before your next period. As mentioned, the luteal phase usually lasts 12-16 days. Your follicular phase can often vary in length from cycle to cycle; by contrast, your luteal phase will be fairly consistent.
If you have visited our online community forum, you may have encountered the acronym, "DPO". This is another way of referring to the luteal phase, it means Days Past Ovulation. When the luteal phase begins, your basal body temperature (BBT) increases in order to provide a more fertile environment for a fertilized egg.
If you do not know whether you have an average or short luteal phase, start by assuming the 14 day average. Follow these steps to detect ovulation. Once you know when you have ovulated, you can start tracking your luteal phase. The number of days from the day after ovulation to the day before your next period is the number of days in your luteal phase.
What to do if you have a short luteal phase
For most women, the luteal phase usually last 14 days, but anywhere from 10 to 16 days is considered normal. If yours happens to be shorter than 10 days, it may be too short for successful implantation to occur. A luteal phase defect or luteal insufficiency occurs when the luteal phase is shorter than normal or when the lining of the uterus is not prepared for implantation. Women who are trying to conceive that have a short luteal phase are often treated with progesterone therapy, and some women have found success with other natural remedies. See below for further information.
When does implantation occur?
Implantation will only occur if an egg becomes fertilized, if a sperm does not penetrate the egg within 12 to 24 hours of ovulation, implantation will not occur during the cycle.
If the egg does become fertilized, it starts dividing and making the slow journey from the fallopian tube to the uterus (about three to four days). Once the fertilized egg reaches the uterus it makes it way to the side wall and implantation begins. This is where the fertilized egg begins burrowing into the plush uterine wall (about 8 days after fertilization). Some women notice slight bleeding or spotting at this time called implantation bleeding.
Luteal phase defect
A luteal phase defect occurs when the luteal phase is shorter than normal or when the lining of the uterus is not prepared for implantation. This may happen if the ovary is secreting lower levels of progesterone than normal or if the lining of the uterus simply is not responding to the normal stimulation of progesterone from the ovary. Given that implantation is a crucial part of early pregnancy, a luteal phase defect can severely impact pregnancy.
Luteal phase defect symptoms
Symptoms of luteal phase defect include: shorter cycles and having periods more frequent, trouble getting pregnant and bleeding.
If your doctor suspects a luteal phase defect, they may assess the endometrial cells of the uterine lining around two days before you are due to menstruate. From here, your doctor can evaluate the quality of your endometrium. Your doctor will also ask you to notify them when you get your period. If the biopsy is taken on day 26 of a 28-day cycle and you get your period two days later, your luteal phase is considered "in phase", or normal. If you get your period on day 27 or after day 29, you will be considered "out of phase" and a luteal phase defect will be diagnosed. Since it is common for women to have a cycle that is off by a day or two, at least two biopsies are usually taken during two or more cycles before a diagnosis can be made.
Luteal phase defect treatment
Your doctor may use clomiphene citrate or human menopausal gonadotropins (hMG) to stimulate follicular growth; supplement with hCG to improve progesterone secretion; or provide you with progesterone supplements, by injection, orally or vaginally after ovulation.
Normal menstrual cycle symptoms
Over the course of a normal menstrual cycle, there are many physical changes that you may notice in your body. These can vary woman to woman and even cycle to cycle, but may include:
- Cramping: Some women experience a slight cramping around the time of ovulation, typically on one side. This is known as mittelschmerz, or middle pain and signals that ovulation is occuring. If you experience cramping, it can be a very helpful indictor when trying to conceive. Do not be alarmed if you have not experienced any form of cramping as not all women will.
- Increased cervical mucus: Near the time of ovulation cervical mucus is released to aid in conception. It not only makes intercourse more enjoyable, but helps facilitate the transportation of sperm through the cervix to find the egg in the fallopian tube. You may notice this increasing until the midpoint of your cycle, which is typically when ovulation will occur.
- Breast tenderness: Some of the hormones involved in your menstrual cycle may cause your breasts to become tender. This is fairly common. Some women will need to wear a bra to prevent their breasts from aching, while others only notice a slight increase in sensitivity.
- Mood swings: As the hormones shift during your cycle, you may also notice that your mood swings too. Some women find that they are very sensitive or emotional in the week before their period is due. This is typically called premenstrual syndrome or PMS. Some women will experience this more than others, while some women will not notice it at all.
- Back pain: Before your period starts, you may notice that your back hurts a bit. This can be a sign that your period is about to start. Other women notice a heavy feeling in their pelvis, or a combination of the two.
- Skin changes: You may also notice that at certain points of your cycle, your skin breaks out with acne. This is not a return to your teen years, but it is caused by your hormones. Typically this is short lived, even if every cycle.
What factors may affect normal menstrual cycle symptoms?
There are many things that might alter your symptoms and how you experience your cycle. This can include the form of birth control that you may be using, other medications, and your general health. If you have any serious changes in your cycles, you should report it to your doctor as it may indicate that you have a problem.